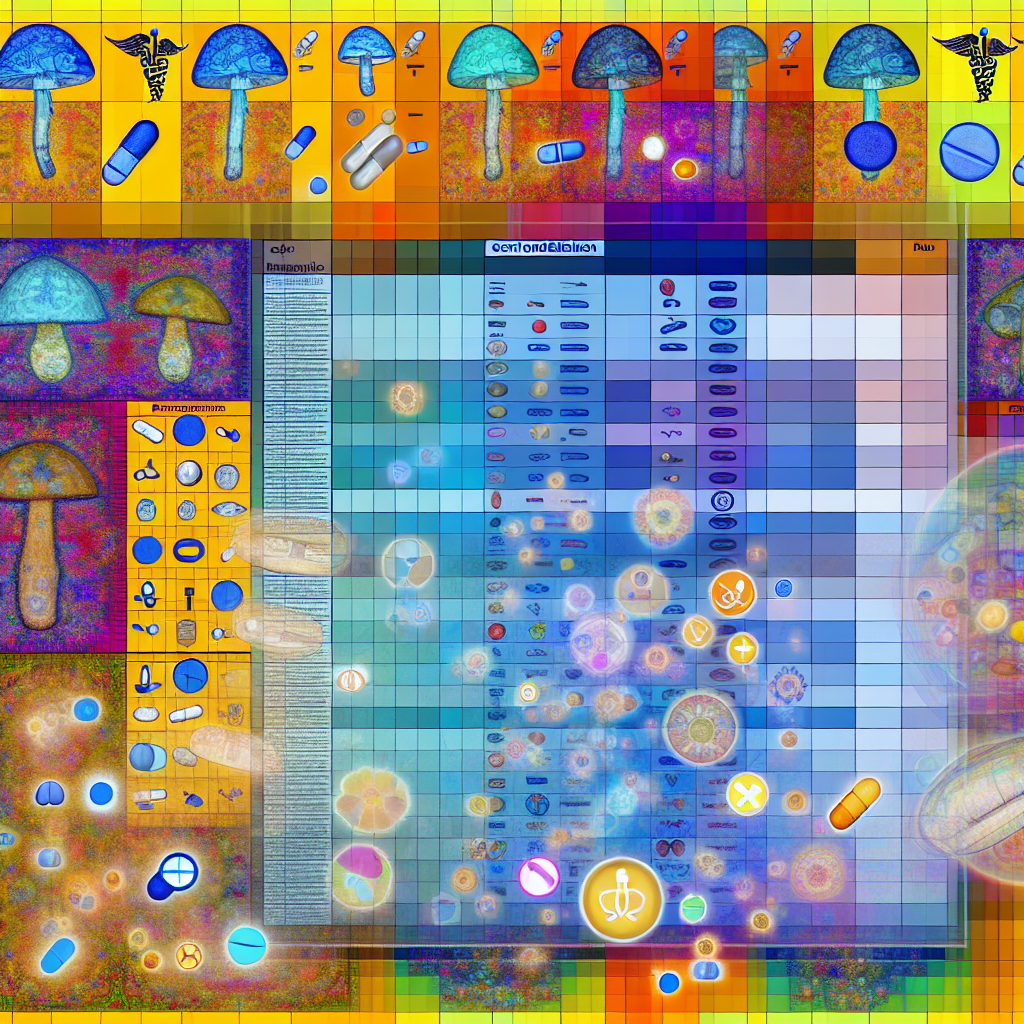
Comprehensive Contraindication Database – Psilocybin and Pharmaceuticals
Introduction
Psilocybin, a naturally occurring psychedelic compound found in hallucinogenic mushrooms, is gaining recognition for its transformative effects in treating mental health conditions such as treatment-resistant depression, anxiety, PTSD, and substance use disorders. Multiple clinical studies support its use where conventional medications often fail by disrupting rigid thought patterns and evoking deep psychological insights.
However, the interplay between psilocybin and traditional pharmaceutical medications raises safety concerns. Psilocybin primarily acts as a 5-HT2A serotonin receptor agonist, creating complex interactions with drugs that affect the same or adjacent neurotransmitter pathways. Co-use with medications like SSRIs, MAOIs, antipsychotics, benzodiazepines, and stimulants can result in a wide range of risks—including serotonin syndrome, emotional blunting, hypertensive crises, and diminished psychedelic efficacy.
There is an urgent need for a centralized resource—a Comprehensive Contraindication Database. Such a system would allow clinicians, facilitators, and patients to cross-reference medications and identify potential interaction hazards. This would guide tapering strategies, ensure safe administration practices, and help build robust risk mitigation protocols as psilocybin moves into therapeutic settings.
As clinical research evolves and jurisdictions move toward legalizing or decriminalizing psychedelics, such a database stands at the intersection of safety, efficacy, and informed decision-making.
Features: Medical Research on Psilocybin-Pharmaceutical Interactions
As clinical and anecdotal data accumulates, a clearer picture is emerging of how psilocybin interacts with various drug classes. Key pharmaceutical categories include:
1. SSRIs and SNRIs (Selective and Serotonin-Norepinephrine Reuptake Inhibitors)
Common SSRIs like fluoxetine (Prozac) and sertraline (Zoloft) increase serotonin availability by blocking its reuptake. Psilocybin, on the other hand, activates serotonin receptors, particularly 5-HT2A. This dual action creates the theoretical risk of serotonin syndrome—a state characterized by agitation, elevated heart rate, tremors, and fever.
More commonly, SSRIs appear to blunt the psychological effects of psilocybin, reducing the depth and transformative capacity of the psychedelic experience. A 2021 study in Psychopharmacology found that users on antidepressants reported fewer mystical-type experiences and weaker therapeutic outcomes during psilocybin-assisted sessions.
Read the full study here:
Psychopharmacology Journal – Interaction Between SSRIs and Psilocybin
2. MAOIs (Monoamine Oxidase Inhibitors)
Drugs such as phenelzine and tranylcypromine inhibit monoamine oxidase, an enzyme critical in breaking down serotonin and psilocybin’s active compound, psilocin. When used together, these drugs can exponentially intensify the psychedelic experience—unpredictably—and increase the risk of serotonin toxicity.
Traditionally, some indigenous entheogenic brews may have included MAOI-containing plants, but these were used in spiritually regimented contexts. Modern usage alongside prescription MAOIs poses much greater danger due to unknown dosages and pharmacological variability.
3. Antipsychotics and Mood Stabilizers
Medications like risperidone, quetiapine (Seroquel), or olanzapine act primarily as antagonists at serotonin receptors, effectively blocking psilocybin’s mechanism of action. This can nullify or significantly diminish the psychedelic experience. Moreover, there’s a documented risk of psychosis in vulnerable populations when combining psychedelics with antipsychotic medications or when tapering poorly.
A 2019 review in Frontiers in Psychiatry cautioned against the use of serotonergic psychedelics in patients at risk for psychosis or mania, particularly when concurrently using other psychiatric medications.
4. Benzodiazepines
Common benzodiazepines like lorazepam (Ativan) and alprazolam (Xanax) are CNS depressants that are sometimes used during psychedelic experiences to mitigate overwhelming emotions. However, chronic use prior to a psilocybin session is known to inhibit emotional processing and dull the potential for meaningful psychological breakthroughs.
While occasionally helpful for managing “bad trips,” routine benzodiazepine use significantly dampens the psychedelic’s therapeutic value. Retreat centers and clinical trials generally advise participants to avoid these medications prior to sessions, underscoring the importance of proper medical planning and tapering.
5. Stimulants and Sympathomimetics
Medications such as Adderall (amphetamine salts) and Ritalin (methylphenidate) elevate dopamine and norepinephrine levels. When used alongside psilocybin, these compounds can overstimulate the nervous system, increasing risks of anxiety, paranoia, and cardiovascular strain.
Although clinical data is still limited, the combination creates predictable risks based on known pharmacodynamics. Individuals with underlying heart conditions or anxiety disorders may be especially vulnerable.
The Role of Tapering and Monitoring
To ensure safety, medical supervision is essential when tapering off medications that may interfere with or complicate psilocybin-assisted therapy. Institutions like Johns Hopkins University and Imperial College London now incorporate medication status as part of their clinical screening.
A pivotal 2020 Johns Hopkins study revealed that individuals who tapered off antidepressants prior to their psilocybin therapy experienced longer-lasting and more significant reductions in depression symptoms compared to those who did not.
The foundation is now laid for a dynamic, continuously updated, evidence-based Contraindication Database that addresses not only contraindicated drugs but tapering durations, interactions by drug class, and the impact of long half-life agents (e.g., fluoxetine) on the psychedelic experience.
Browse more from the Imperial College London Psychedelic Research Centre.
Conclusion
As psilocybin continues forging its way into legitimate clinical and therapeutic frameworks, the need for caution is unified with the push for innovation. A centralized, scientifically vetted contraindication database stands as a vital safeguard. It empowers patients, therapists, and healthcare providers to engage in this healing modality with grounded understanding and risk awareness.
Only through informed practices, sound tapering protocols, and continued interdisciplinary research can psilocybin’s healing potential be fully realized—transforming mental health treatment for future generations.
Concise Summary
Psilocybin shows great promise in treating mental health conditions, but combining it with common pharmaceuticals may lead to adverse effects such as serotonin syndrome, cardiovascular stress, or therapeutic blunting. SSRIs, MAOIs, antipsychotics, benzodiazepines, and stimulants pose specific interaction risks. Research indicates that tapering medications before psilocybin therapy enhances outcomes. A centralized Contraindication Database is essential to ensure safety, guide clinical protocols, and support informed choices as psilocybin treatment becomes more mainstream.
References
– Psychopharmacology: Interaction Between SSRIs and Psilocybin
– Frontiers in Psychiatry: Risks of Psychedelic Use in Those With Psychosis
– Johns Hopkins Study on Psilocybin and Depression (2020)
– Imperial College London Psychedelic Research Centre

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives. Film Student and Full-time Medical Writer for ContentVendor.com