Psilocybin + Transcranial Magnetic Stimulation – Combined Protocol for Treatment-Resistant Depression (TRD)
Introduction
In recent years, the convergence of **psychedelic therapy** and **neurostimulation techniques** has created promising new pathways for addressing complex mental health conditions like **treatment-resistant depression (TRD)**. TRD, a severe subtype of **major depressive disorder (MDD)**, is characterized by persistent symptoms even after trying at least two standard antidepressants.
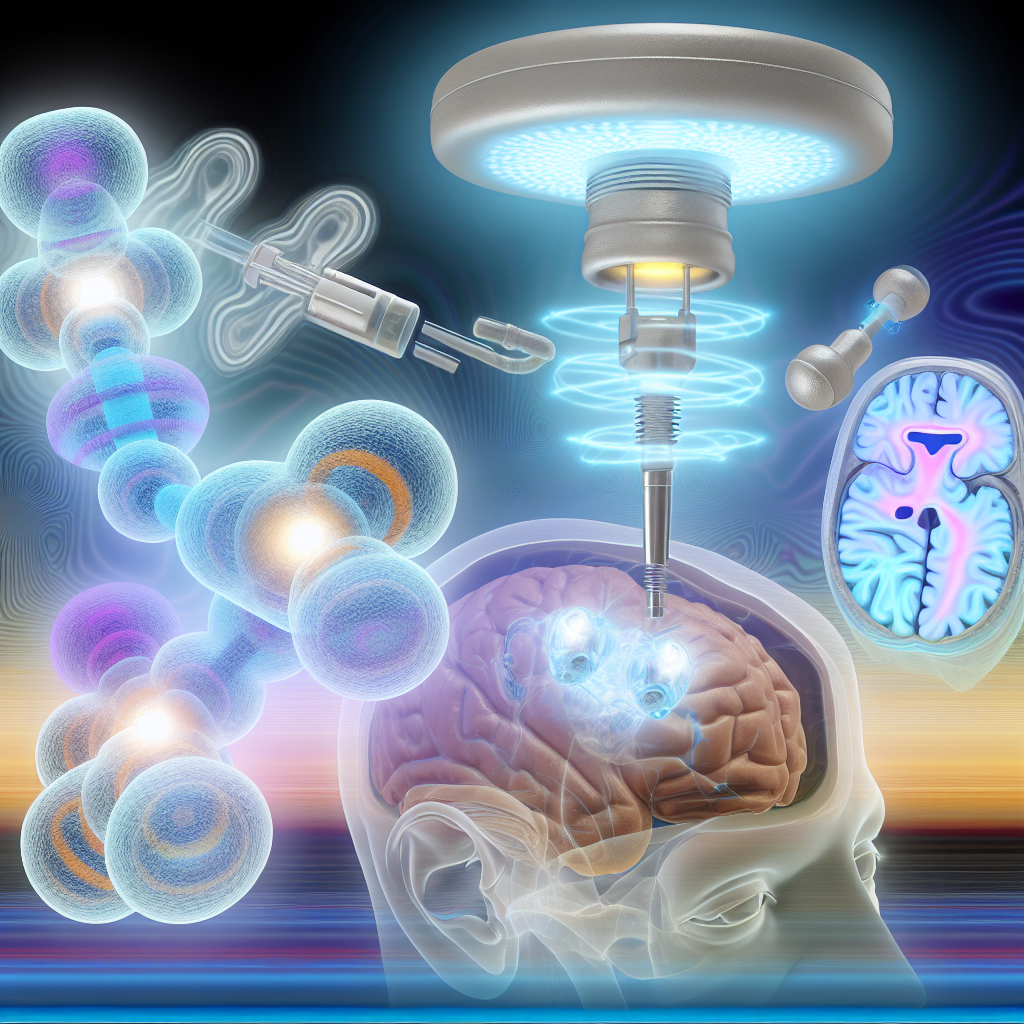
This condition poses ongoing challenges in clinical practice, often requiring innovative strategies beyond conventional medication. Among the most exciting are therapeutic approaches involving **psilocybin**, the psychoactive compound in psychedelic mushrooms, and **Transcranial Magnetic Stimulation (TMS)**, a non-invasive neurological treatment that modulates brain activity through magnetic fields.
Psilocybin has re-emerged in psychiatric research due to its ability to rapidly reduce depressive symptoms after just one or two sessions in supportive clinical settings. Acting primarily on the **serotonin 5-HT2A receptor**, psilocybin induces a transient but profound alteration in consciousness that supports **emotional insight, cognitive flexibility**, and mental reset.
Meanwhile, TMS, approved by the FDA since 2008, provides a physical intervention by delivering focused **magnetic pulses** to stimulate **mood-regulating brain regions**, particularly the **dorsolateral prefrontal cortex (DLPFC)**.
What makes the current research groundbreaking is the hypothesis that a combined protocol—administering TMS during or shortly after the plasticity window opened by psilocybin—could result in more durable, reinforced changes in brain circuits, with potentially transformative outcomes for TRD patients.
Features and Medical Studies
The fusion of **psilocybin therapy and TMS** rests on the compelling scientific foundation that both modalities promote **neuroplasticity**, but do so via complementary mechanisms.
Psilocybin, according to a landmark 2021 study published in the New England Journal of Medicine (Carhart-Harris et al.), demonstrated efficacy comparable—and in some measures superior—to escitalopram, a leading SSRI, in reducing depressive symptoms. Notably, this effect was achieved with just two doses, emphasizing the medicine’s potential for rapid, lasting relief.
In addition to subjective symptom reduction, **neuroimaging research** indicates that psilocybin disrupts overactive brain circuits like the **Default Mode Network (DMN)**, commonly associated with rumination and negative self-focus in depression. By promoting temporary disintegration of the DMN, psilocybin increases global brain connectivity, allowing for cognitive and emotional reframing.
TMS has a well-defined therapeutic profile. Meta-analyses, such as the one by Sackeim et al. published in the Journal of Affective Disorders (2020), report response rates of 50-60% and remission in about 30% of TRD patients. It is unique in its ability to **target specific brain areas non-invasively** and is typically associated with fewer side effects compared to pharmacological approaches.
What draws special attention is their potential synergy. A 2022 pilot study by Zhang et al. in Frontiers in Psychiatry explored the administration of TMS 24-48 hours after a psilocybin session. The goal was to take advantage of the **“plasticity window”**—a period during which the brain is more receptive to reorganization and change. Findings suggested enhanced mood stability, prolonged antidepressant effect, and fewer anxiety relapses in the weeks that followed.
Moreover, both treatments appear to increase **brain-derived neurotrophic factor (BDNF)**, a critical neurotrophin involved in neuronal growth, resilience, and synaptic connectivity. Animal models show that psychedelics robustly increase BDNF expression; this is mirrored by BDNF upregulation seen with TMS protocols as well. Whether additive or synergistic, this biochemical overlap is a key rationale behind dual-modality treatment.
Organizations such as the Multidisciplinary Association for Psychedelic Studies (MAPS) and the Johns Hopkins Center for Psychedelic and Consciousness Research are on the forefront of exploring the integration of psychedelic substances with technological enhancements like TMS. These ventures—not yet mainstream—are laying the groundwork for FDA-sanctioned investigational trials.
With ongoing developments in neurotechnology and psychedelic medicine, this integrative protocol may not only alleviate symptoms but also correct underlying network dysfunctions at the core of TRD.
Conclusion
For patients grappling with **treatment-resistant depression**, conventional therapies often fall short. The emerging **combined protocol of psilocybin and Transcranial Magnetic Stimulation** promises a more holistic and durable intervention. Rooted in well-established scientific principles and supported by early data, this dual approach could mark a paradigm shift in how we understand and treat psychiatric disorders.
By exploiting the neuroplastic state induced by psilocybin—followed by strategic neural reinforcement using TMS—this protocol may offer a deeper reset, not just symptom alleviation but transformation of the underlying mental architecture. As clinical studies evolve and larger trials commence, this innovative blend of ancient compounds and modern engineering may forge a new frontier in mental healthcare.
Concise Summary
Psilocybin combined with Transcranial Magnetic Stimulation (TMS) is emerging as a cutting-edge protocol for treating treatment-resistant depression (TRD). Psilocybin, a serotonin receptor agonist, induces profound emotional insight and cognitive flexibility, while TMS non-invasively stimulates mood-related brain circuits. When timed correctly, TMS applied post-psilocybin may enhance and solidify the therapeutic gains of the psychedelic experience. Research indicates this synergy benefits from overlapping boosts in neuroplasticity and BDNF expression. While still early in development, the combined protocol offers hope for TRD patients and is under active investigation by leading research institutions.
References
– Carhart-Harris, R. L., et al. (2021). Trial of Psilocybin versus Escitalopram for Depression. The New England Journal of Medicine.
– Sackeim, H. A., et al. (2020). The Clinical Efficacy and Safety of Transcranial Magnetic Stimulation (TMS) in Depression: A Systematic Review and Meta-Analysis. Journal of Affective Disorders.
– Zhang, Y., et al. (2022). Combining Psychedelic Therapy with Transcranial Magnetic Stimulation: A Novel Approach for Treatment-Resistant Depression. Frontiers in Psychiatry.
– Multidisciplinary Association for Psychedelic Studies (MAPS). Research Publications.
– Johns Hopkins Center for Psychedelic and Consciousness Research.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives. Film Student and Full-time Medical Writer for ContentVendor.com